Blog
A Step in the Right Direction: What New Glycemic Clinical Outcomes Beyond HbA1c Mean for Hospitals
Imagine if a patient’s blood glucose was still determined through urine strip testing. Although it was once seen as a best practice, it would now be laughable and likely thought of as downright poor patient care. As medicine evolves, the best practices and guidelines must continuously be reviewed and updated to account for the current evidence-based and state-of-the-art knowledge. In the diabetes community, this is exactly what occurred with the new consensus statement published in the journal Diabetes Care, “Standardizing Clinically Meaningful Outcome Measures Beyond HbA1c for Type 1 Diabetes.” The statement recognizes glycemic management outcomes other than just hemoglobin A1c (HbA1c) and clearly defines measurements.
HbA1c, a measure of mean blood glucose over the course of three months, has long been used as the primary outcome associated with glycemic management and used by payers and others for determination of and evaluation of therapies, technology and care reimbursement. However, more clinicians have realized there are limitations to focusing only on this one measure. HbA1c does not capture short-term variations in blood glucose or episodes of hypoglycemia and hyperglycemia that can have a significant negative impact on one’s health. To fully capture glycemic management, additional outcomes need to be measured, which led the JDRF to organize a steering committee comprised of representatives from eight leading diabetes organizations including, the American Association of Clinical Endocrinologists, the American Association of Diabetes Educators, the American Diabetes Association, the Endocrine Society, JDRF International, The Leona M. and Harry B. Helmsley Charitable Trust, the Pediatric Endocrine Society, and the T1D Exchange.
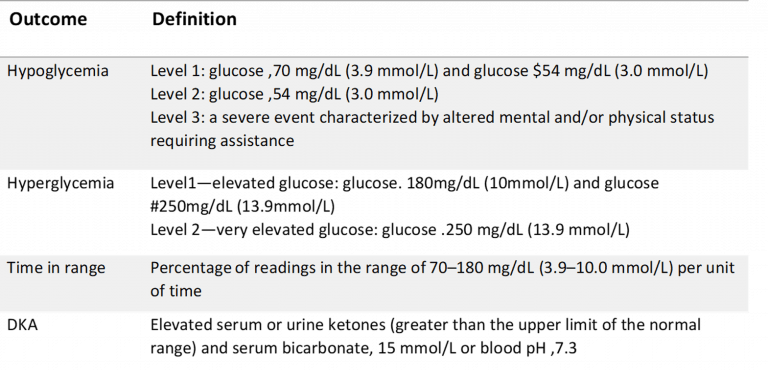
The effort, which began two years ago, considered research and the opinions of leading industry experts as well as patients with diabetes to develop the new consensus statement. The steering committee concluded that the other clinically meaningful outcomes that should supplement HbA1c to determine the efficacy of diabetes therapies, treatments, and technologies should now include hypoglycemia, time in normal range, hyperglycemia and diabetic ketoacidosis (DKA). They also established clear definitions for these measures outlined in the table below.
What This Means for Hospitals
Although the consensus was not specifically tied to inpatient care and focuses on type 1 diabetes, it does pave the way for standardizing consistency of glycemic management metrics across institutions and all patients. Hospitals should be tracking episodes of hypoglycemia, hyperglycemia, time in range, and DKA, if they are not already doing so, to understand how they are performing. To solve their glucose management challenges and improve patient outcomes, numerous hospitals are moving to electronic glycemic management systems like EndoTool, which have shown to improve patient safety even in complex and challenging patient cases such as DKA.
In addition to standardizing metrics, the consensus also provides a basis for value-based reimbursement approaches, and ultimately a framework for better clinical care. Within the hospital, hyperglycemia is linked to increased risk of infection, slower wound healing, longer length of stay, and poor patient outcomes. Hypoglycemia is even more of a threat with severe hypoglycemic events associated with increased mortality. With initiatives in place to address and improve these priority outcomes, including precise, patient-specific insulin dosing recommendations, hospitals can provide better care for patients and better perform under new reimbursement models. It is expected that the new consensus will bring more patient safety and payer-related scrutiny to glucose management and glucose metrics of in-hospital patients.
Overall, the latest consensus statement is a step in the right direction. It is providing evidence-based guidelines to help to continue to evolve and improve glycemic management and deliver better patient care. For hospitals, that means reducing hyperglycemia, while avoiding hypoglycemia.
Related posts
Blog
Preparing for CMS Glycemic Reporting: A Quality Leader’s Perspective
Preparing for CMS Glycemic Reporting: A Quality Leader’s Perspective
Blog
2026 Marks a Shift: Glycemic Safety Is No Longer a Clinical Preference, It Is a System Requirement
2026 Marks a Shift: Glycemic Safety Is No Longer a Clinical Preference, It Is a System Requirement
Blog
Creating a Culture of Confidence: Supporting Nurses Through Change
Creating a Culture of Confidence: Supporting Nurses Through Change
Get in Touch
Ready to get started?
"*" indicates required fields